In the third trimester of pregnancy, the baby’s brain architecture and neural circuits rapidly mature. During this crucial period, the baby’s brain is highly vulnerable to many factors, such as the activation of the mother’s immune system. Maternal immune activation (MIA) releases several chemical substances, some of which affect the baby’s developing brain.
When Is the Mother’s Immune System Activated?
The mother’s immune system is activated in response to infection, stress, poor physical health, and inflammation. Several classes of proteins are released to stimulate the immune response. Two of the most frequently released proteins are interleukin-6 (IL-6) and C-reactive protein (CRP).
Maternal immune activation has been studied in many preclinical studies involving rodents and nonhuman primates. These studies suggest that MIA interferes with the development of brain circuitry and associated behaviors, which may increase the risk of psychiatric illness in offspring.
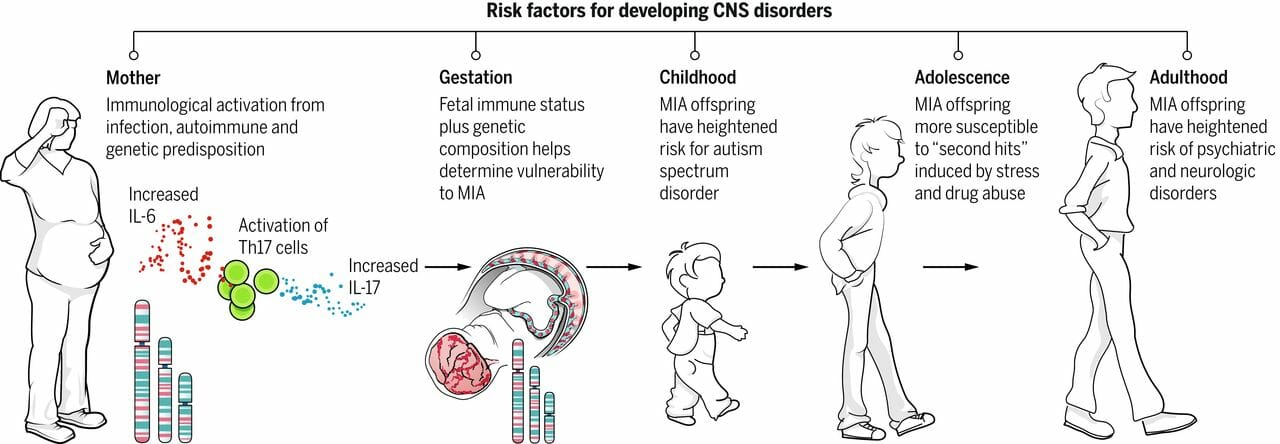
This schematic depicts the current model for how MIA leads to psychiatric disorders in offspring. Infection leads to the release of pro-inflammatory cytokines and the activation of TH17 cells in the mother’s bloodstream. A combination of genetic background, autoimmune status, and second hits during childhood and adolescence (including stress and drug abuse) impact the consequences of maternal infection and increase the likelihood that offspring will develop psychiatric disorders as adults. Image Source: SemanticScholar (Estes, Myka L., and A. Kimberley McAllister. “Maternal Immune Activation: Implications for Neuropsychiatric Disorders.” Science 353, no. 6301 (2016): 772–777.)
MIA is believed to alter the development of widespread and nonspecific regions of the brain, including the hippocampus, prefrontal cortex, mid-temporal lobe, parietal lobe, cingulate cortex, and insula. These regions are associated with memory and learning, cognition and behavior, hearing, language, and emotion processing. Any alteration in the development of these regions may increase the risk of psychiatric disorders, such as autism spectrum disorder (ASD) and attention deficit hyperactivity disorder (ADHD).
Does the Maternal Immune System Really Alter Fetal Brain Development?
In a study titled “Maternal Immune Activation during the Third Trimester Is Associated with Neonatal Functional Connectivity of the Salience Network and Fetal to Toddler Behavior,” researchers from the United States studied the relationship between MIA and fetal brain development in terms of IL-6 and CRP levels in the blood. This study revealed important connections between fetal brain development and MIA.
Adolescent pregnant women between the ages of fourteen and nineteen years old were recruited for the study. The participants received routine prenatal care and did not experience any pregnancy complications.
The researchers assessed fetal heart rate (FHR) at thirty-four to thirty-seven weeks of gestation. Blood samples were drawn to determine the levels of IL-6 and CRP in the mothers’ blood. After birth, the researchers obtained MRI scans of the babies’ brains to check for neural connectivity. At fourteen months of age, the infants’ cognitive, motor, and language skills were assessed.
Results
Maternal levels of CRP and IL-6 correlated with the babies’ brain development and fetal heart rate. The type of delivery also correlated with maternal IL-6 levels. The mothers who had C-sections had the highest levels of IL-6. The mothers who had spontaneous vaginal deliveries had moderate levels of IL-6. The mothers who had assisted vaginal deliveries had the lowest IL-6 levels.
In terms of neural connectivity, higher IL-6 and CRP levels were associated with better connectivity in some parts of the brain, but in other parts of the brain, higher levels of IL-6 and CRP seemed to cause weaker connectivity. The infants born to mothers with higher IL-6 and CRP levels showed better cognitive development at fourteen months of age. Researchers hypothesize that improved cognitive development is due to the better neural connectivity associated with higher levels of IL-6 and CRP. On the contrary, the brain regions that suffered from weaker connectivity may be the cause of psychiatric disorders in offspring.
Higher maternal CRP levels also caused a decreased fetal heart rate, which typically increases from the second to the third trimester. A faster FHR during this time is a predictor of better cognitive development at two and two and a half years of age, and it is necessary for the development of the autonomic nervous system (ANS). The findings suggest that MIA may slow fetal ANS development, leaving the child vulnerable to long-term neurodevelopmental outcomes.
Thus, mothers should refrain from stressful activities and situations during pregnancy and take better care of their bodies. In cases of infection or inflammation, mothers can take medicines to cure themselves. However, an activated immune system may still affect the baby’s rapidly developing nervous system, and the effects may be long-term and uncurable.
Reference
Spann, Marisa N., Catherine Monk, Dustin Scheinost, and Bradley S. Peterson. “Maternal Immune Activation during the Third Trimester Is Associated with Neonatal Functional Connectivity of the Salience Network and Fetal to Toddler Behavior.” Journal of Neuroscience 38, no. 11 (2018): 2877–2886. Retrieved from http://www.jneurosci.org