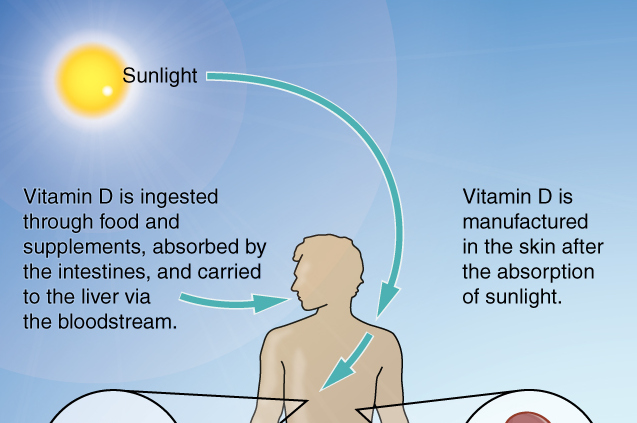
It is important to supplement the maternal diet with certain vitamins, such as vitamin B12, during pregnancy and lactation. But in some areas, especially in underdeveloped countries, vitamin supplements are not available, and women cannot acquire them due to a lack of economic resources.
In particular, vitamin B12 deficiency is common among people from low- and middle-income countries, especially in women and children whose animal-source food consumption is limited.
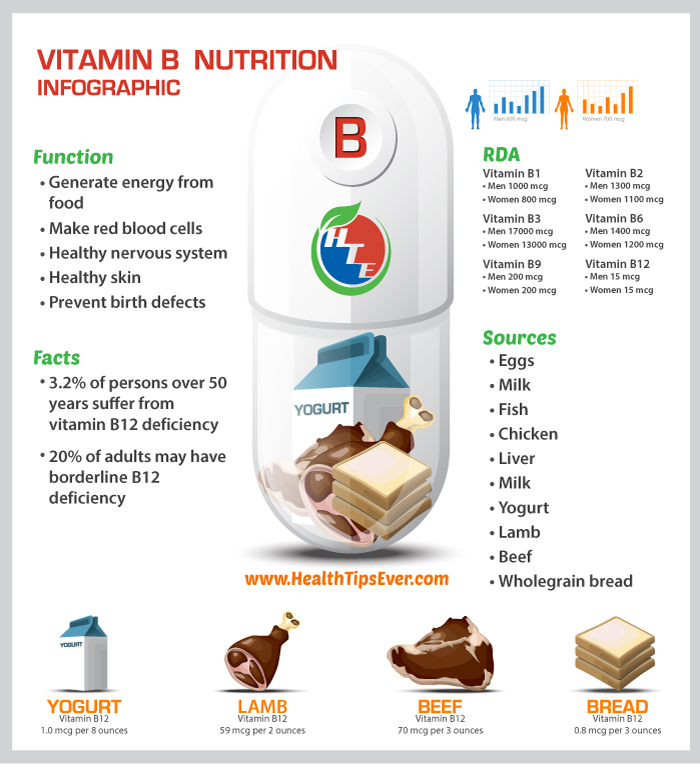
Since vitamin B12 is primarily found in animal-source foods and the economic conditions in many countries limits the consumption of these foods as well as the availability of vitamin supplements, it is likely that children of mothers who live in these nations will suffer from vitamin B12 deficiency and other clinical conditions.
Vitamin B12 deficiency is associated with some cases of anemia and insulin resistance. The risks for infants born to mothers with low levels of vitamin B12 include metabolic disorders, developmental delays, failure to thrive, and poor growth. Infants are particularly vulnerable to vitamin B12 deficiency because infancy is a period of rapid growth.
A Research Study
Some researchers from California traveled to Kenya and performed a study titled “Vitamin B-12 Concentrations in Breast Milk Are Low and Are Not Associated with Reported Household Hunger, Recent Animal-Source Food, or Vitamin B-12 Intake in Women in Rural Kenya.” The main objectives of the study were to measure vitamin B12 levels in breast milk and examine its association with household hunger and recent animal-source food and vitamin B12 intake in rural Kenyan mothers.
Data on dietary intake and breast milk samples were collected from three hundred women participating in a previous trial designed to evaluate the efficacy of improved nutrition, water quality, sanitation, hygiene, or combined practices on child growth and development.
These samples were later analyzed to calculate the mean vitamin B12 concentration in the breast milk and other important information. Some mothers’ demographic characteristics were also assessed, such as BMI (calculate BMI here), prenatal visits, marital status, level of education, age, householder hunger score, and animal-source food score. All of these variables were important for further analysis.
Findings
The mean concentration of vitamin B12 in the breast milk was much lower than what is considered normal by the World Health Organization (WHO). Only 11 percent of the milk samples showed vitamin B12 levels that would be considered acceptable or normal.
Seventy percent of the women did not meet their estimated calorie intake requirement. Around 60 percent of the mothers consumed less vitamin B12 during lactation than the estimated average requirement.
There were no significant connections between vitamin B12 concentration in breast milk and household hunger score, animal-source food score, maternal BMI, birth location, season, or maternal education.
Low vitamin B12 concentrations were prevalent in the breast milk of the study population, which suggests that both the mothers and the infants suffer from vitamin B12 deficiency. The median vitamin B12 concentration in this breast milk would have provided an exclusively breastfed infant with an amount of vitamin B12 far below what babies require.
Conclusion
Many mothers in rural areas are unable to purchase sufficient amounts of animal-source food; therefore, dietary recommendations for pregnant and lactating women in Kenya coupled with nutritional education may not be enough to improve the quality of the maternal diet. For women experiencing hunger, effective supplementation strategies are necessary to improve vitamin B12 status. These strategies must be carried out by the government and local authorities in order to be successful.
Despite these findings, researchers insist that the best food for babies is breast milk. They recommend that mothers breastfeed as long as possible while also focusing on improving their diets.
Consult a doctor before changing an existing routine or starting any new intervention during pregnancy.
Reference
Williams, Anne M., Caroline J. Chantry, Sera L. Young, Beryl S. Achando, Lindsay H. Allen, Benjamin F. Arnold, John M. Colford Jr et al. “Vitamin B-12 Concentrations in Breast Milk Are Low and Are Not Associated with Reported Household Hunger, Recent Animal-Source Food, or Vitamin B-12 Intake in Women in Rural Kenya–4.” The Journal of Nutrition 146, no. 5 (2016): 1125–1131. Retrieved from https://academic.oup.com/jn